Article
What is a bio-decontamination system?
Nov 29, 2022
Sunil Ingle
EHS General Manager
Biological cleaning is essential in any setting where tissue and microorganisms are processed. This can include everything from hospital departments to research institutes.
A facility may need to be decontaminated regularly at predetermined periods. Ensure that it maintains a clean-air environment.
Employees frequently introduce contamination through the natural shedding of hair or skin particles during their employment, necessitating regular cleaning. However, following a specific contamination incidence, the process may need to be completed as soon as possible.
What Is Bio-Decontamination? What Are The Different Methods Of Bio-Decontamination?
Bio-decontamination, also known as biological decontamination, is a unique procedure of eliminating or minimizing the presence of various biological contaminants such as fungi, viruses, bacteria, or several other microorganisms, from a climate setting, setting, or object. It is a critical process in numerous areas, which includes pharmaceuticals, healthcare, laboratory research, biohazard response, and food processing.
Bio-decontamination intends to prevent the spread of infectious diseases, ensure the safety of the environment & individuals and maintain sterile situations. It generally includes the utilization of specialized methods and agents to destroy or inactivate the target microorganisms in an effective manner.
There are a lot of various methods of bio-decontamination, and each & every one of them is suitable for specific requirements and situations. Some of the common methods are mentioned below:
a) Chemical Decontamination — This encompasses the utilization of sterilants, disinfectants, or antimicrobial agents to neutralize or kill microorganisms. Some instances of generally utilized agents encompass chlorine compounds, hydrogen peroxide, ethylene oxide, and quaternary ammonium compounds.
b) Radiation Decontamination — There are specific types of radiation such as ionizing radiation or ultraviolet light, that can be used to damage or destroy microorganisms. UV light is generally utilized for surface decontamination while ionizing radiation might be applied for larger-scale decontamination in technological facilities.
c) Heat Sterilization — Heat can be utilized to attain decontamination via various methods such as autoclaving, which utilizes high-pressure steam in order to kill microorganisms. It is extremely effective for heat-resistant substances.
d) Biological Decontamination Systems — Some of the advanced systems such as aerosolized hydrogen peroxide and hydrogen peroxide vapor help in generating and distributing a fine stream of hydrogen peroxide via an enclosed region in order to eliminate biological contaminants. All these systems are generally utilized in controlled environments such as laboratories or clean rooms.
Routine Decontamination
Various environments necessitate regular bio-cleaning as best practice at specific intervals. These are some of them:
● Healthcare: Sanitation and sterilization are required regularly in isolation rooms and critical care wards, as well as operating theaters, blood banks, and other facilities with a high standard of cleanliness. To avoid any risk of infection for patients and workers, sterilization is also required following the treatment of specific disorders. In addition, a bio-decontamination system is required in test labs that routinely test for infections to avoid risk to the operators' health.
● Research: Animal research facilities and cleanrooms or labs processing pathogenic materials, such as those where medical problems and illnesses are researched, must meet the highest standards. This is necessary not just for operator safety but also to maintain the integrity of study findings and ensure that they are not tainted by contamination.
● Facilities for Pharmaceuticals and Biotechnology: These institutions must maintain sterility at all times and have cleanrooms and laboratory facilities. It's critical to protect the quality of the pharmaceuticals and other materials being handled and the safety of the employees.
Cleanroom testing, monitoring, biological sampling, and validation are all services that should be coupled with routine laboratory or hospital decontamination. If you follow a routine that includes all of these, you'll soon notice any chronic issues that aren't resolved by regular cleaning or filtration and must be handled.
Emergency Decontamination
Decontamination will be performed as part of regular cleanroom maintenance and testing visits as part of the contract. Cleanrooms and other facilities, on the other hand, may require one-time sterilization in the event of a specific problem.
This could be due to a leak of a known pathogenic or contaminating chemical or a malfunctioning piece of equipment that poses a danger of contamination. There could have been an unexpected incidence of a pathogen or exceptionally pathogenic substance detected by monitoring systems, or there could have been a suspicion or discovery of unusually high contamination levels.
Water spills or floods can contaminate a cleanroom, lab, or operating theater, and a power loss and subsequent equipment failure can also result in airborne pollution. Another reason for a contamination notice could be a one-time occurrence, such as a staff member being ill.
There could be contamination in an unmonitored region near a cleanroom or clean lab and difficulties in the cleanroom or clean lab itself. In a public space or an unsupervised general laboratory within a facility, there may be a sign of an alarm, but the type or extent of contamination is unknown.
In all of these situations, it's a good idea to call in a skilled cleanroom service crew for an emergency visit. If the source of the contamination is unknown, they will conduct testing in the region to diagnose the issue and make any necessary repairs. The facility can then be decontaminated and rapidly put back into use, saving time and money.
What Is The Difference Between Sterilization And Bio-Decontamination?
Sterilization is any chemical or physical technique that kills all living things, particularly microorganisms (including bacteria and bacterial spores) and inactivates viruses. As a result, the terms "sterile" and "sterilization" refer to the absence of all live germs and their elimination.
Bio-decontamination is removing or reducing microbiological contamination to an acceptable level. For the periodic cleaning of critical environments, many techniques and antimicrobial agents have been used. However, these procedures are difficult to standardize, time-consuming, and possibly harmful to employees and the environment.
Wiping off surfaces with antimicrobial solutions is time-consuming, and it gets difficult to standardize the process. Spraying, fogging, or fumigation procedures are commonly used to disinfect laboratory animal rooms and temperature-sensitive (non-autoclavable) objects, especially formaldehyde-based chemicals.
Traditional formaldehyde fumigation may be helpful, but it is time-consuming, difficult to standardize, and disruptive, not to mention hazardous and carcinogenic. For these reasons, authorities have been rigorously regulating the use of formaldehyde for some years.
Fumigant
Description
Advantages
Disadvantages
Formaldehyde
Heating formalin or paraformaldehyde added to potassium permanganate crystals produces a liquid or aerosolized formalin or formaldehyde gas.
Inexpensive
Broad-spectrum efficacy claimed.
Long exposure times and slow reaction.
Surface residues can build up and be difficult to remove.
The mode of action is cross-linking. Toxic, carcinogenic, and a strong irritation
Pre-cleaning of surfaces is required.
High humidity is required for efficiency. This is not an automated system.
Vaporized Hydrogen Peroxide ("'Dry')
During pre-set control cycles, the system produces and administers vaporized hydrogen peroxide, preventing condensation on a target surface.
Rapid
Validated
Broad-spectrum efficacy has been published. Compatibility of materials
Degrades quickly into water and oxygen. A process that is automated and controlled
Cosmetic material may be affected on the surface
It's a good idea to clean the surfaces ahead of time.
Doesn't work well with materials that are highly absorbent (e.g. cellulosic)
A bio-decontamination system based on vaporized hydrogen peroxide (VHP) was developed in the 1980s and commercialized in the early 1990s. Since then, this technique has grown in prominence. It is now utilized to decontaminate clean rooms, animal rooms, ambulances, big-volume filling rooms, and hospital wards infected with antibiotic-resistant microorganisms.
VHP is a strong oxidant that can inactivate viruses, bacteria, fungi, nematode eggs, bacterial spores, and even prions. The VHP technique is quick, dry, portable, electronics-compatible, and effective at low concentrations and temperatures.
In addition, VHP, unlike formaldehyde, creates harmless by-products (water and oxygen), making it environmentally friendly and eliminating the need for post-process neutralization and cleaning. However, a VHP concentration of over 75 ppm is considered an immediate risk to human health; the accepted personal exposure level is under 1 pp.
Safe, automated decontamination methods are being more widely used as an alternative to formaldehyde because of their ease of use, higher levels of sterility assurance, and overall cost savings to a facility. Vaporized hydrogen peroxide (VHP) has been used widely to sterilize pharmaceutical applications, including production filling lines, sterility testing environments, sealable enclosures, production rooms, and lyophilizers.
In addition, this method has recently been applied to decontaminating animal rooms as an alternative to formaldehyde. Compared to formaldehyde, hydrogen peroxide vapor is a broad-spectrum antimicrobial with virucidal, bactericidal, fungicidal, and sporicidal activity.
Furthermore, the procedure has no environmental risks associated with formaldehyde because the vapor easily breaks down into water and oxygen.
The creation and maintenance of hydrogen peroxide vapor in an enclosed environment is the basis of the VHP decontamination procedure. Because the hydrogen peroxide vapor concentration is kept below the condensation (or dew) threshold, VHP decontamination is virtually 'dry,' with excellent material compatibility. The effectiveness of vapor-phase hydrogen peroxide in a pass-through box for decontaminating possibly contaminated equipment and inanimate items with exotic animal viruses was tested.
Representatives of numerous virus families (Orthomyxoviridae, Reoviridae, Caliciviridae, Paramyxoviridae, Flaviviridae, Picornaviridae, Herpesviridae, and Rhabdoviridae) from both avian and mammalian species were tested. The gas's effects on various laboratory equipment were also investigated. Virus suspensions were dried on glass and stainless steel from cell culture media, egg fluid, and blood. Virus viability was measured after 30 minutes of exposure to vapor-phase hydrogen peroxide.
The decontamination process reduced the virus titer to 0 embryo-lethal doses for avian viruses (avian influenza and Newcastle disease viruses) and less than 10 tissue culture infective doses for mammalian viruses for all viruses tested and under all conditions (except one) (African swine fever, hog cholera, bluetongue, swine vesicular disease, pseudorabies, vesicular exanthema, and vesicular stomatitis viruses).
The laboratory equipment that was exposed to the gas appeared to be unaffected. In biocontainment level III laboratories where exotic animal disease virus agents are handled, vapor-phase hydrogen peroxide decontamination can be advised as a safe and effective method of eliminating possibly virus-contaminated materials.
Let us discuss some available bio-decontamination systems in the market -
VHP 1000 Bio-decontamination System.
The VHP 1000 Bio-decontamination System (STERIS Corporation, Mentor, Ohio) is a small, mobile device that produces and controls VHP delivery into an enclosed space. Dehumidification, conditioning, decontamination, and aeration are the four steps of the cycle.
The relative humidity is lowered to 10% to 30% during dehumidification by circulating the air in a closed loop. VHP is created during conditioning by vaporizing 31 percent or 35 percent liquid hydrogen peroxide and then introducing it into the recirculating air stream to quickly attain the necessary VHP concentration.
Finally, the decontamination phase follows the same steps as the conditioning phase but at a constant injection and recirculation flow rate to keep the VHP concentration constant for the duration of the exposure. Unlike the liquid, the vapor is sporicidal at low concentrations (typically 1 to 2 mg/L in vapor at 25°C) (4), and the concentration is kept constant by continuously introducing VHP into the incoming air and catalytically degrading VHP present in the returning air during the programmed exposure cycle.
Finally, VHP is not injected during aeration following decontamination, and the leftover vapor is catalytically dissolved into water and oxygen by recirculating through the destroyer or using the room ventilation system. The VHP 1000 microprocessor automatically monitors and/or regulates the process parameters during each cycle.
While aqueous hydrogen peroxide (H2O2) has long been used to disinfect inanimate surfaces, vapor-phase hydrogen peroxide (VPHP) as a gaseous disinfectant is still relatively recent. In the past, formaldehyde or ethylene oxide was used to disinfect equipment and heat-sensitive materials that couldn't be treated any other way.
These glasses are highly effective, but they are poisonous, carcinogenic, and possibly explosive, necessitating strict handling techniques and extensive ventilation periods for ethylene oxide. VPHP is a safe alternative to using these harmful gasses and the necessity to neutralize them before releasing them into the atmosphere. In addition, VPHP degrades to oxygen and water, both harmless to the environment.
Bacteria, yeasts, fungi, viruses, and spores are all susceptible to aqueous hydrogen peroxide. However, data is inadequate on the efficacy of VPHP, and its activity against exotic animal viruses is unknown. VPHP has the potential to be used in laboratories and research institutions to decontaminate heat-sensitive laboratory equipment.
For example, in a biocontainment level III laboratory, all materials must be effectively decontaminated before leaving the facility. This can be an issue for things that cannot be autoclaved or passed through a liquid-disinfectant tank. In pass-through boxes used to disinfect materials leaving the laboratory, VPHP could be a valuable fumigant.
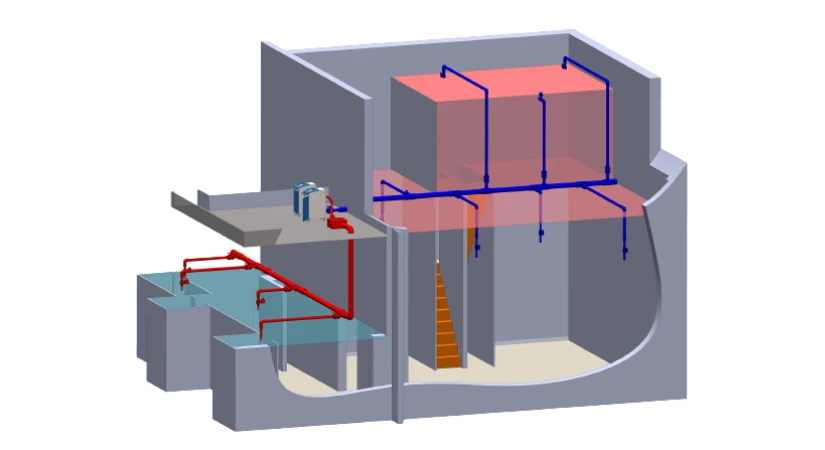
Bioreset: Innovative hydrogen peroxide V-Phase bio-decontamination solutions
Bioreset is primarily used to eliminate airborne and surface microbiological contamination in regulated or classified environments for pharmaceutical, biomedical, biotechnological, animal care, and any other microbiologically sensitive environment.
Bioreset is efficient and quick, requiring no pre-conditioning of the environment, employs Hydrogen Peroxide (H2O2), and is low-maintenance. Bioreset is the most cost-effective solution on the market because of the speed of the cycles and the lack of expensive consumables.
Microbiological contamination must be controlled for manufacturing and research to fulfill the required quality and safety standards.
To maintain the necessary conditions and manage the hazards of microbiological contaminants prevalent in these environments, VPHP bio-decontamination cycles should be performed regularly.
Bioreset is a bio-decontamination technology that uses cold sterilization with Vapour-Phase Hydrogen Peroxide. It kills all known microbes, is chemically active against spores with confirmed kill rates, and is easier to handle and employ than other gaseous agents.
What Are The Applications Of Bio-Contamination?
Bio-decontamination has various applications in multiple industries, here are some of the common applications of bio-decontamination:
1) Healthcare Facilities — Bio-decontamination plays a vital role in clinics, hospitals, and various healthcare facilities. It assists in controlling the spread of infections and makes sure that a safe environment for visitors, patients, and healthcare workers. Bio-decontamination methods are utilized to disinfect the rooms of patients, isolation units, operating theaters, and various medical equipment.
2) Pharmaceutical Industry — The pharmaceutical industry needs certain stringent cleanliness standards to assure the efficacy & safety of drug manufacturing. The techniques of bio-contamination are enforced to sterilize production places, equipment, clean rooms, and storage facilities. This helps in avoiding contamination of drugs as well as maintains quality control.
3) Laboratory & Research Facilities — Laboratories and research facilities generally deal with hazardous biological samples and agents. Bio-decontamination is utilized to sanitize laboratory tools & equipment, animal research facilities, biosafety cabinets, and other regions where biological experiments are performed! It helps to protect researchers, avoids cross-contamination, and maintains the integrity and virtue of experiments.
4) Food Processing And Packaging — Bio-decontamination is crucial in the food and packaging industry in order to prevent the development and spread of toxic/harmful microorganisms. It is utilized to sanitize packaging substances, processing equipment, and food storage regions. Effective bio-decontamination techniques provide assurance of the safety and augmented shelf life of food products.
5) Cleanrooms And Controlled Environments — Industries such as aerospace, electronics, semiconductor manufacturing, and precision engineering depend on cleanrooms and controlled environments in order to maintain the product's quality. Bio-decontamination is crucial in these settings to eliminate microbial contamination and conserve strict cleanliness standards.
In Conclusion
That’s it on bio-decontamination systems. We hope you found this article useful and informative. Do you have any doubts about bio-decontamination? Then do share them with us right away.